A research team made up of scientists from the National Eye Institute (NEI), a branch of the National Institutes of Health (NIH), has used patient stem cells and 3D bioprinting to produce eye tissue that the team says will advance understanding of the mechanisms of blinding diseases.
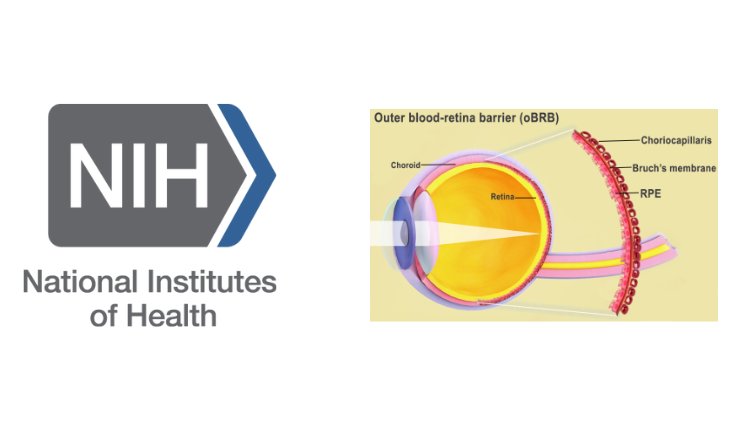
The researchers printed a combination of cells that form the outer blood-retina barrier, eye tissue that supports the retina’s light-sensing photoreceptors. According to the team, the technique provides a theoretically unlimited supply of patient-derived tissue to study degenerative retinal diseases such as age-related macular degeneration (AMD).
“We know that AMD starts in the outer blood-retina barrier,” said Kapil Bharti, Ph.D., who leads the NEI Section on Ocular and Stem Cell Translational Research. “However, mechanisms of AMD initiation and progression to advanced dry and wet stages remain poorly understood due to the lack of physiologically relevant human models.”
Bharti and the team combined three immature chorodial cell types in a hydrogel: pericytes and endothelial cells, which are key components of capillaries; and fibroblasts, which give tissues structure. The hydrogel was then printed on to a biodegradeable scaffold, and days later the cells began to mature into a capillary network.
On day nine of the experiment, the scientists seeded retinal pigment epithelial cells on the flip side of the scaffold. The team says the printed tissue reached full maturity on day 42. According to the researchers, analysis and genetic and functional testing showed that the printed tissue looked and behaved similarly to native outer blood-retina barrier.
“By printing cells, we’re facilitating the exchange of cellular cues that are necessary for normal outer blood-retina barrier anatomy,” said Bharti. “For example, presence of RPE cells induces gene expression changes in fibroblasts that contribute to the formation of Bruch’s membrane, something that was suggested many years ago but wasn’t proven until our model.”
Co-author on the study, Marc Ferrer, Ph.D., director of the 3D Tissue Bioprinting Laboratory at NIH’s National Center for Advanced Translational Sciences said: “Our collaborative efforts have resulted in very relevant retina tissue models of degenerative eye diseases. Such tissue models have many potential uses in translational applications, including therapeutics development.”
In August 2022, researchers based in Hyderabad, India, successfully 3D printed an artificial cornea and transplanted it into the eye of a rabbit.